A study published in the NCBI indicated that autoimmunity affects about 5-8% of the population, including both men and women. These usually arise from complex interactions among genetic susceptibility, immune dysregulation, and environmental triggers. Approximately 80 disorders, including rheumatoid arthritis, lupus, multiple sclerosis, and Hashimoto’s thyroiditis, can be categorized as autoimmune disorders. These disorders are known to cause chronic inflammation and damage bodily tissues and were earlier considered irreversible. Well, newer research published in Springer Nature indicates the possibility of autoimmune activity becoming reversible.
To help you understand the science behind what these disorders are and how to reverse autoimmune disease, this article synthesizes current scientific evidence to outline ten strategic, mechanism-based approaches that help support long-term remission within a comprehensive, integrative framework.
Comprehensive Overview of Autoimmune Reversal
Autoimmune diseases arise from immune dysregulation influenced by genetics, environment, and lifestyle. Evidence shows symptoms can improve through targeted interventions like anti-inflammatory diets, gut microbiome support, vitamin D optimization, stress management, exercise, restorative sleep, toxin reduction, and personalized functional medicine. Addressing root causes rather than symptoms enhances immune regulation, reduces inflammation, and supports long-term remission. Dr. David Bilstrom’s practice specializes in creating tailored, science-based protocols for sustained immune health and symptom relief.
What Is Autoimmune Disease?
An autoimmune disease is one of the many disorders in which the immune system targets the body’s own cells, tissues, or organs, losing self-tolerance, causing inflammation, and ultimately deteriorating the body. Some autoimmune diseases are specific to one part or system of the body, while others affect the entire bodily system. These disorders are influenced by genetic predisposition, immune regulation, and environmental factors. Symptoms vary widely depending on affected systems and disease severity over time.
Can Autoimmune Disease Be Reversed?
Autoimmune diseases were always considered chronic and incurable till date. Well, are they actually not reversible? The answer is no! Many top autoimmune doctors, such as Dr David Bilstrom, suggest that autoimmune symptoms can be reversed and managed easily with the right medicinal and nutritional approach. In fact, a study published in Science News Today showed evidence that suggests autoimmune disorders can be significantly reduced and, in some cases, driven into sustained remission.
Here, “reversal” does not typically mean eliminating genetic susceptibility. It simply stems from the fact that immune dysfunction is dynamic and influenced by modifiable factors such as gut microbiome composition, nutrient status, metabolic health, environmental exposures, stress signaling, and sleep. This means that targeted dietary interventions, reduction of inflammatory triggers, correction of immune imbalances, and lifestyle optimization can improve symptoms, normalize biomarkers, and reduce medication dependence in certain patients. Outcomes vary by condition, timing, and individual biology.
To gain deeper insights on this topic, listen to Dr David Bilstrom’s discussion on reversing autoimmune conditions on The Ultimate Health Podcast, where he explains the science, clinical strategies, and patient outcomes in detail. You can access the episode here!
10 Strategies to Reverse Autoimmune Disease
Here are some proven strategies on how to reverse autoimmune diseases:
1. Anti-Inflammatory Diet
Diets that focus on reducing inflammation, like the Mediterranean or AIP (Autoimmune Protocol) diets, advocate for the consumption of whole foods and healthy fats, as well as unsweetened, processed food-free vegetables, and lean proteins. Increased consumption of whole foods and healthy fats has been associated with reduced inflammatory biomarker levels and improved immune response in patients with autoimmune or chronic inflammatory disease.
2. Gut Microbiome Support
Randomized trials published in BMC Medicine have shown that gut microbiota-based therapies (probiotics, prebiotics, and tailored diets) can positively affect disease activity and immune markers in several autoimmune diseases. A balanced microbiome supports intestinal barrier integrity and reduces systemic immune activation.
3. Personalized Elimination & Nutrition
Dietary modifications tailored to individual immune responses (e.g., eliminating gluten, dairy, or other triggers) can alter antigen exposure and reduce immune stimulation. These have been linked to favorable changes in gut microbiota and immune responses in autoimmune disease contexts.
4. Vitamin D Optimization
Vitamin D influences immune regulation by modulating T and B cell responses and supporting tolerance mechanisms. Higher serum vitamin D levels have been associated with reduced risk of certain autoimmune diseases and improved immune function, though dose responses vary by individual and condition.
5. Regular Moderate Physical Activity
Regular, moderate exercise supports immune homeostasis, reduces chronic inflammation, and enhances overall health without triggering excessive stress responses. Physical activity can improve the quality of life and decrease inflammatory cytokines that help reverse autoimmune disease conditions.
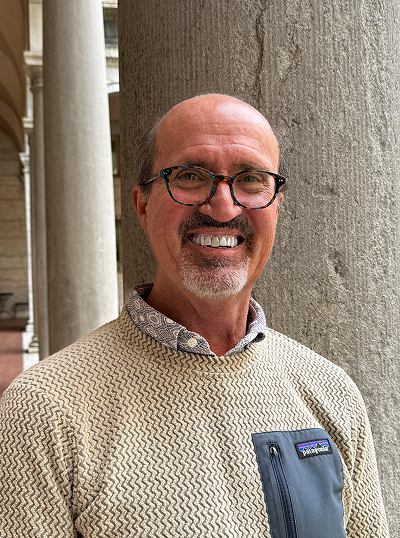
5. Stress Management
Chronic stress disrupts hormonal and immune balance, often exacerbating autoimmune flares. Techniques like mindfulness, meditation, yoga, and deep breathing have been shown to lower cortisol and support neuroimmune regulation.
6. Sleep Quality & Circadian Balance
Adequate sleep (7–9 hours nightly) supports immune regulation and reduces pro-inflammatory signals. Sleep disturbances can amplify stress responses and disrupt immune balance, making restorative sleep a core component of autoimmune management.
7. Targeted Supplementation
As discussed some micronutrient supplements (like vitamin D at moderate doses) show potential immune benefits. But the list doesn’t stop here. Research published in the NCBI suggests specific fats like omega-3s and adequate antioxidant intake help lower inflammation and immune activation when personalized to individual needs, thus helping reverse autoimmune disorder symptoms.
8. Environmental & Toxin Reduction
Chronic exposure to environmental toxins (such as BPA, phthalates, and pollutants) can contribute to immune dysregulation. Minimizing exposures through cleaner products, filtered water, and lowered household chemicals may reduce immune burden and inflammatory triggers.
9. Comprehensive Functional Medicine Assessment
A personalized, root-cause functional medicine approach, including evaluation of gut function, lifestyle, hormones, nutrient status, and toxin exposures, can identify underlying contributors to immune dysfunction and tailor multi-modal protocols that go beyond symptom suppression.
For those seeking practical guidance on reversing autoimmune conditions, Dr. David Bilstrom offers in-depth insights in his podcast. He explains functional medicine approaches, like diet, gut health, stress reduction, and lifestyle optimization, backed by science. Watch the episode here: Autoimmune Functional Medicine Podcastand start your journey to better immune health today.
Conclusion
Reversing autoimmune diseases cannot simply be addressed through sporadic methods; it requires a tailored, evidence-based approach that deals with the underlying problems associated with each autoimmunity. With a specialty in the Functional Medicine Protocols, Dr. David Bilstrom offers a unique combination of nutritional, lifestyle, and targeted therapy-based approaches to help restore the health of the immune system. Begin your path to sustained immune health and relief from autoimmune symptoms by contacting us for assistance in developing your personalized autoimmunity treatment plan today!
Frequently Asked Questions
Functional medicine autoimmune doctors diagnose and manage autoimmune diseases, depending on the organ system affected and symptom patterns.
Yes, by addressing root causes, optimizing nutrition, lifestyle, and gut health, functional medicine may reduce flare frequency, potentially lowering reliance on long-term medications under supervision.
Some infections may prompt immune responses that mimic self‑tissues, potentially initiating or worsening autoimmune reactions in genetically susceptible people.
Yes, having one autoimmune condition increases the likelihood of developing additional autoimmune disorders over time.
Autoimmune conditions are generally more common in women and can occur at any age, with some types more prevalent in children or older adults.